Most of the time when you hear judgment being leveled on the success, or failure, of the so-called “war on drugs” the focus tends to be related to the illicit drug market and the impact on people and communities affected by it. Defenders of drug control, whether it be national police officials or international regulators, tend to cite statistics on quantities of drugs seized, opium or coca crops eradicated, and the numbers of people incarcerated for committing drug crimes to illustrate the persistence of the problem and the ongoing need for aggressive counter-narcotic action. Critics often cite the same statistics, however they do so to highlight the violent and devastating impact that policing of drug “crimes” has had especially on poor and minority communities even while, historically, the war itself has not led to any substantial reduction in the scale or scope of the illicit drug market—in fact quite the opposite.
These critics rightly point out that the ‘war on drugs’ has been a resounding failure even when measured by its own stated goal – violence, dangerous consumption, and political instability all seem to be perpetually on the rise in contexts where the drug war receives the largest amounts of funding.
What receives much less attention, but perhaps should in fact be at the heart of debates about the value of drug control, is another resounding failure of the current drug regulatory regime, namely, its incapacity to ensure peoples’ access to essential medicines. Maybe talking about the availability of medicine is not as sexy as tales of drug busts, gangster culture or police bravado, but nevertheless the international conventions which govern drug control actually have enshrined within them a dual purpose: one, to prevent the diversion of licit drugs into illicit circuits, and two, to ensure the availability of controlled medicines for medical and scientific purposes. The International Narcotics Control Board (INCB), the body responsible for monitoring and helping governments to enforce this regulatory imperative, describes this objective in the following terms: “Governments need to meet the dual objective of the international drug control treaties, namely, preventing the diversion and abuse of internationally controlled substances while ensuring their availability for legitimate use.”
In 2010 the INCB issued a special supplement to the Board’s annual report that focused on the “availability of internationally controlled drugs” and that outlined the abysmal gap between the developed and developing world in terms of access to what the World Health Organization (WHO) identifies as “essential medicines.” There are many medicines that are deemed essential yet are woefully out of the reach of the majority of the world’s population. The narcotic drugs, opiates in particular, are among the most easily tracked—because of the system of international control which requires countries to submit annual statistics on production, import, export, and consumption. Opiates are indispensable to modern medicine (a fact undisputed by all the regulatory agencies involved in drug control) and are particularly valued for the alleviation of pain. The lack of access to adequate pain medication for an estimated 80% of the world’s population has been receiving an increasing amount of attention. Echoing the concern expressed by the INCB, the World Health Organization this year released a report on “access to controlled medicines” which points out that the general lack of access to opiates for pain relief undermines basic human rights guaranteed both by its own constitution and by the Universal Declaration of Human Rights: “The overall result is lack of access to adequate pain treatment and the denial of the human right to access the highest attainable standard of health, and the right not to be subject to torture or to cruel, inhuman or degrading treatment or punishment.” While the consumption of opiates as prescribed painkillers increased five fold over the last twenty years, the rise has happened primarily in the developed world. According to the INCB, 90 percent of global consumption occurred in Australia, Canada, New Zealand, and the United States, with the U.S. and Canada having by far the highest levels of consumption in the world. In most countries availability is “low or inadequate”, and as the Board points out, the level of access and consumption is “generally correlated with its level of socio-economic development.” In other words, a not surprising yet important fact is that the majority of the world’s poor population is desperately lacks access to basic medical care.
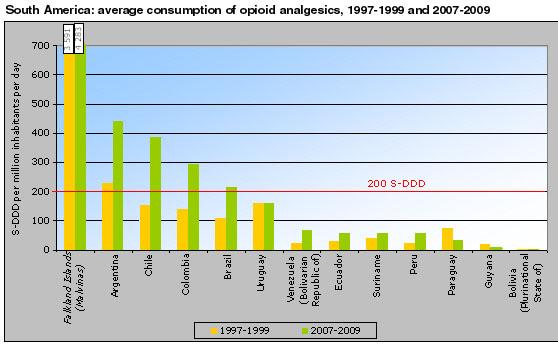
[This chart shows the average consumption of painkilling opiates in South America. The WHO has devised a statistical measure whereby any country falling under 200 S-DDD (an estimated defined daily dose needed for a million people per day) is considered to be inadequate in its provision of this essential medicine.]
There are a number of reasons identified for the huge disparity in the global provision and availability of these valuable drugs. The INCB emphasizes the lack of medical training and misplaced concern that consuming these painkillers is liable to produce dependence or abuse as major factors preventing wider dissemination of the drugs (even while warning that in countries where there is a super-abundance, like the United States, there is a growing problem of their diversion into illicit circuits.) The Board also recognized other factors that the WHO identified as the most critical: the highly inflated retail price of painkilling medication in the developing world, the common approach to opioid consumption as a criminal justice problem rather than a health problem, and, significantly, the obstacles established by the drug control system itself. For a country to gain access to supplies of opioid medicines it must comply with international and national drug control regulations which produce an onerous burden on officials in developing countries often working under less than ideal circumstances which make it often impossible to effectively comply with the preconditions established by the international system of drug control before gaining legitimate access to these medicines: tracking the domestic market, licensing manufacturers, distributors, and doctors, coordinating import and export authorizations with a producing country to guarantee a supply, and reporting on production, importation, exportation, and consumption to the INCB. The drug control system itself rather than ensuring access to critical medicines, as the WHO points out, often limits the availability of essential medicines despite the desperate need for such medicines among people all over the world.

